TB STILL A MAJOR HEALTH PROBLEM
Sunday, 24 March 2013 | Nitindra Bandyopadhyay | Chandigarh
Rate : 0/5
Like : 0
Tuberculosis is the
second major cause of death due to a single infectious agent after HIV/AIDS. In
India it is a major public health problem affecting nearly three million people
in 2011 says Dr Vineet Saggar, Spinal Surgeon Ivy Hospital.
According to studies, TB death rate from 1990 to 2009 has
dropped from 42 per 1,00,000 to 23 per 1,00,000 respectively. The disease
burden is still huge along with its associated socio-economic challenges.
In order to mark the significance of raising awareness about the
prevention and management of this pervasive disease, which often turns fatal.
World Tuberculosis Day is celebrated globally each year on March 24.
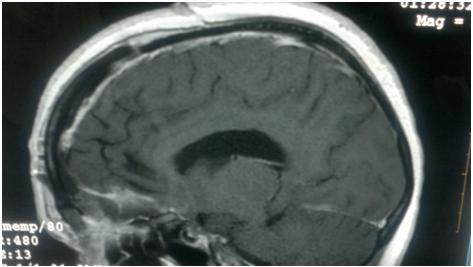
TB, which is caused by the bacteria Mycobacterium tuberculosis,
is preventable as well as curable.
Although pulmonary infection, which affects the lungs, is the
most common type, the TB bacteria can affect other organs and tissues of the
body as well, like the brain, lymph glands, stomach, bones and spine or the
backbone.
Spinal tuberculosis is predominantly a disease of the young, the
usual age of manifestation being the first three decades of life, thereby
affecting people in their most productive years.
The diagnosis of spinal tuberculosis is difficult and it
commonly presents at an advanced stage. Spinal tuberculosis progresses
gradually and the early manifestations, like back-ache, fever, weakness, weight
loss, nausea and vomiting, are often not paid heed to or are mistaken for other
health problems, leading to its diagnosis at much advanced stages says the
expert.
Though the mainstay of treatment in patients of spinal
tuberculosis is Anti Tubercular treatment but surgery is required in cases of
neurological deficits due to vertebral collapseor epidural abscess, infact
acute vertebral collapse or epidural abscess causing cord compression are
surgical emergencies , adds Dr Saggar.
World Tuberculosis Day brings an opportunity to draw attention
towards innovations in medical technology made over the period of last 20
years, bringing efficacy and safety in complicated surgical procedures like
spine surgeries, making treatment of spine injuries easier and quicker.
Dr. Vineet Saggar (MCh)
Neuro Surgeon / Spinal Surgeon
Chandigarh, Mohali -
Ivy Hospital Sector 71
+91-9855990990http://www.neurosurgeoninchandigarh.com
http://neurosurgeonhead.blogspot.in/
http://www.facebook.com/neuro.surgeon.7186
http://www.slideshare.net/neurosergeonheadNeuro Surgeon / Spinal Surgeon
Chandigarh, Mohali -
Ivy Hospital Sector 71
+91-9855990990http://www.neurosurgeoninchandigarh.com
http://neurosurgeonhead.blogspot.in/
http://www.facebook.com/neuro.surgeon.7186